Should You Have an MRI? A Comprehensive Guide
Many patients often ask, “Do I need an MRI?” Deciding to have an MRI isn’t just a random choice; specific criteria guide this recommendation. In this article, I’ll dive into the circumstances in which doctors might advise an MRI.
1. Recognizable Symptoms:
Doctors typically suggest an MRI for individuals when they notice the following:
- Pain that spreads to a limb.
- Sensations of numbness or tingling.
- A consistent increase in weakness in the affected area.
2. Monitoring Treatment Progress:
If you’re undergoing treatment for a condition and you don’t observe any improvement, or if your symptoms persist for a long duration, then considering an MRI becomes relevant.
Take, for instance, a patient who displays foot weakness alongside sciatica symptoms. They might skip the MRI if they show a positive response to therapy in a few weeks. On the other hand, if they don’t see any relief in pain or gain in strength, then proceeding with an MRI becomes a logical course of action.
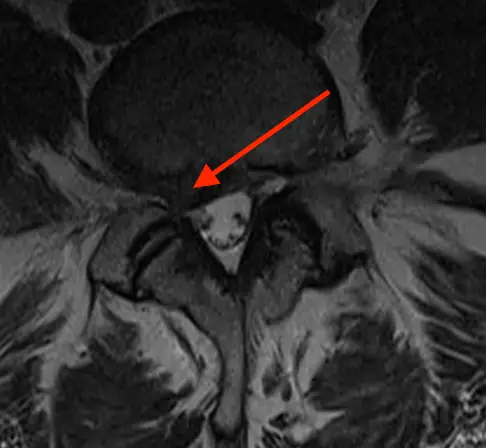
3. Uncovering Disc Herniation:
One primary purpose of MRI referrals is to identify disc herniation, a condition where the disc applies pressure on the nerves. Upon detecting this, a patient often consults a GP for specialized attention.
4. Disc Tears or Fissures:
Sometimes, individuals suffering from sciatic pain don’t exhibit typical symptoms like numbness or weakness. In these instances, doctors aim to detect a possible fissure or minute tear in the disc. Encouragingly, these tears often heal by themselves with time
5. Addressing Concerns for Young Athletes:
An MRI proves essential for young athletes experiencing acute lower back pain that intensifies when arching the back. Here, the objective is to inspect for any inflammation or fluid accumulation in the vertebra’s pars interarticularis. Doctors strongly advise restricting such athletes’ activities for a few months. Doing so helps avert the onset of a stress fracture termed spondylolysis, a condition that becomes permanent once established.
6. Heeding Other Warning Signs:
Occasionally, symptoms like abrupt weight loss, mysterious lymph node swelling, fever paired with back pain, or bladder/bowel disturbances may signal the need for an MRI. Furthermore, while solo headaches might not commonly call for an MRI, the scenario changes if they pair up with symptoms like intensifying pain, seizures, personality transitions, sudden bouts of vomiting, one-sided body debility, or walking issues.
In Conclusion:
We always prioritize our patient’s health and wellness. Therefore, we recommend an MRI only when it aligns with your medical journey.